The ACL (recently also abbreviated as LCA) stands for “anterior cruciate ligament.” It is a very strong internal ligament of the knee, and injuries to it are commonly seen in athletes (both professional and recreational), with recovery often being lengthy and complex.
Anterior Cruciate Ligament Rupture (LCA/ACL)
Description
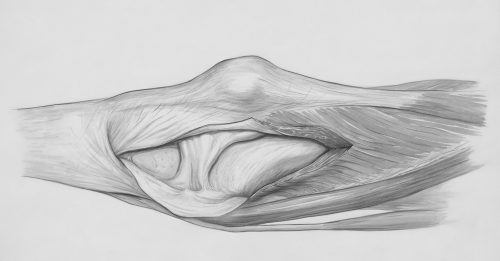
To understand the importance of this ligament in the knee joint system, it’s essential to note that the joint socket in the largest joint in the human body (the knee) is very shallow, while the head resembles a cylinder. This shape allows for high mobility, but it also makes the entire system very unstable and prone to injury.
To reduce the risk of “slipping” of the joint components from their natural positions, the knee is surrounded by several levels of protection. The first are the muscles, which around the knee are the strongest in the body. Then there is a network of external ligaments that surround the joint and provide additional stability. Finally, there are two internal ligaments buried deep within the knee itself, known as the anterior and posterior cruciate ligaments. The ACL prevents the head of the joint from “slipping” forward during numerous movements, both in sports and non-sporting activities.
The mechanism of ACL injury, or rupture, involves trauma that directs external forces to the knee, forcing it into excessive bending and rotation. Examples include falls while skiing, landing in volleyball, changing direction during a handball attack, or even blows or blocking of the lower leg while the body is still in motion (such as in martial arts or sliding tackles in soccer).
 Typically, an ACL injury is accompanied by intense pain, rapid swelling, and reduced knee mobility. For first aid, it is helpful to use cold or ice packs to reduce pain and apply compression with an elastic bandage to minimize swelling. Afterward, an accurate diagnosis of the injury is necessary.
Typically, an ACL injury is accompanied by intense pain, rapid swelling, and reduced knee mobility. For first aid, it is helpful to use cold or ice packs to reduce pain and apply compression with an elastic bandage to minimize swelling. Afterward, an accurate diagnosis of the injury is necessary.
During the first examination, a doctor may attempt to aspirate (evacuate) the swelling from the joint with a needle and syringe. Finding blood in the joint is the first indication that an ACL rupture may have occurred. Removing blood from the knee generally reduces pain and accelerates recovery from the injury. Afterward, knee tests are conducted, and a working diagnosis is made, which is typically confirmed with an MRI scan. MRI imaging shows not only the ligaments but also the condition of all other knee structures. Unfortunately, an ACL rupture is rarely the only injury in the knee. Given the interconnected structures in the joint and the significant forces involved, additional damage to other knee structures, most commonly the meniscus, collateral ligament (one of the knee’s outer ligaments), sometimes cartilage, and less frequently the posterior cruciate ligament (PCL), may occur in the process.
Once the diagnosis of an ACL rupture is confirmed, treatment follows, which is never simple or short. If the ligament is partially torn, a non-surgical treatment approach is used, involving physical therapy and kinesiotherapy. The goal is to reduce any present swelling, gradually strengthen the muscles around the knee, and prepare them for what lies ahead, especially if the patient is an active athlete. This process takes a minimum of 12 weeks and includes techniques to improve endurance, reaction speed, and balance.
For complete ACL ruptures, the situation is more complex, as the ligament cannot simply be “sewn” back together. Since it serves as a crucial stabilizer of the knee, modern orthopedics aims to perform an ACL reconstruction as early as possible. This surgical procedure involves taking a portion of the patellar ligament, part of the quadriceps tendon, or the tendons of two hamstring muscles, and implanting them in place of the ruptured ACL. The seriousness of this procedure is underscored by the fact that both the thigh bone (femur) and shinbone (tibia) are drilled to anchor the ends of the new ligament in prepared channels, secured with implants.
After surgery, a lengthy rehabilitation process follows, which lasts 9 months and includes all elements of the non-surgical treatment for partial ruptures. It’s worth noting that the success rate of this procedure ranges from 70% to 90%, depending on study authors. Success is defined as patients being able to return to their full range of physical activity as they had before the surgery (including athletes).
An alternative to surgery exists, which involves non-surgical treatment aiming to strengthen the muscle-ligament system to compensate for or completely take over knee stabilization. The benefit of this approach is avoiding a rather extensive surgery, and total treatment time is reduced to about 3–4 months. However, there is a risk that if the knee “gives out” again, or becomes unstable during movement, it will likely cause additional damage to other knee structures (like the meniscus, cartilage, or other ligaments). Therefore, the pros and cons of surgery should be weighed carefully for each case, and a treatment plan should be agreed upon with a well-informed patient.
Regarding indications, contraindications, optimal surgical techniques, the ideal age for the procedure, risk factors, and potential complications, so many scientific papers have been written that, if printed, they would fill a large house. To simplify this vast amount of information, it is essential to understand two physiological facts. First, the ACL has no “helper,” meaning that once it is torn, the knee remains unstable. There are two types of instability. One is manifest, presenting as a sensation of the knee “giving out” during daily or sports activities, even after physical therapy and rehabilitation, and is an absolute indication for surgery. The second is micro-instability, which occurs below the sensory threshold, so the patient is unaware of it. It poses a risk for further cumulative damage to the cartilage and other knee structures and is a relative indication for surgery.
The patient’s age is another important factor. Up to 30 years of age, every rupture is an absolute indication for surgery, as micro-instability leads to a high risk of early osteoarthritis, which is challenging, if not impossible, to treat adequately. Between ages 30 and 40, the decision to operate depends on the condition of the knee and the patient’s physical activity level. After age 40, surgery is optional for patients whose activities don’t involve jumping or sudden direction changes and who don’t experience manifest instability, as surgery no longer prevents early osteoarthritis. However, in exceptional cases, knee stabilization surgery can be performed even after 60.
In summary, consult with your orthopedic surgeon and physical therapist to evaluate the pros and cons of both treatment approaches in your case, and choose the path that best suits your needs.
The postoperative rehabilitation protocol can be simplified and expressed in weeks. The total treatment lasts 9 months. Previously, it lasted 6, but we have found that each additional month in which the athlete does not return to full training but continues with guided recovery reduces the rerupture rate by half. This effect is lost after the 9th postoperative month.
The protocol is as follows: 6+6+12+12 (weeks).
In the first 6 weeks, the main goal is to achieve full extension, or straightening, of the knee. The duration of brace wear and crutch use during this period depends on the type of surgery and the protocol of the healthcare facility where the surgery was performed and does not affect the final treatment outcome.
In the next 6 weeks, the primary goal is to establish a normal walking pattern and achieve full knee flexion, or bending.
Over the following 12 weeks, the goals are to restore strength, endurance, and reflex speed (proprioception).
The last 12 weeks are reserved for specific preparations for returning to sports.
Before returning to sports, it is important to test the knee’s capability for athletic activity. In orthopedics, we usually consider isokinetic testing as the most important (this measures the strength of the knee extensors and flexors and their balance). However, simply regaining strength does not mean the knee is stable and ready for sports. That is why, in our clinic, we perform a full battery of tests, which vary from sport to sport, to gain a deeper and broader picture of the knee’s overall readiness and the athlete’s preparedness for the demands of sports activity.
Finally, there is a fact that we are all inclined to overlook: an operated knee is not a new knee. It can be a good knee, but it remains a knee with special needs. The body perceives surgery as another trauma, and even after a sufficiently long and thorough rehabilitation, there is a tendency for the body to weaken the thigh muscles, especially the quadriceps, due to active, old evolutionary reflexes. This means that regular performance of individual preventive exercises, as well as periodic testing, is an important part of preventing both ligament re-injury and damage to other knee, hip, and ankle structures. This preventive work must be carried out as long as the knee is exposed to intense sports activities.
The tension model used in our clinic clearly establishes that knee stability does not depend only on the strength and reaction speed of the muscles surrounding the knee joint. The knee is just one part of a large kinetic chain that includes the entire lower limb and torso, and its movements during running, jumping, and even walking are only one component in the complex system of the entire body. Thus, dynamic stabilization also depends on the condition of all other components of this large kinetic chain. We pay special attention to this fact when rehabilitating patients with an anterior cruciate ligament rupture.