In the 1990s, almost all groin pains, especially in athletes, were attributed to muscle strains or inflammation of their tendons.
Hip impingement syndrome (FAI, femoroacetabular impingement)
Description
 This was a time when soft tissue imaging technology was in its start. Ultrasound was unavailable and of low resolution, and even the only MRI machine in Rijeka at that time, with a strength of ½ Tesla, was not of great help. Furthermore, X-ray findings specific to this syndrome, which will be discussed later in the text, were considered variants of normal anatomy. It wasn’t until the 2000s that the profession began to speak more in detail about this specific problem, and with the development of diagnostic systems alongside our better understanding of the kinematics of this large joint, it gave us precise tools for its recognition and treatment.
This was a time when soft tissue imaging technology was in its start. Ultrasound was unavailable and of low resolution, and even the only MRI machine in Rijeka at that time, with a strength of ½ Tesla, was not of great help. Furthermore, X-ray findings specific to this syndrome, which will be discussed later in the text, were considered variants of normal anatomy. It wasn’t until the 2000s that the profession began to speak more in detail about this specific problem, and with the development of diagnostic systems alongside our better understanding of the kinematics of this large joint, it gave us precise tools for its recognition and treatment.
Simply put, impingement means pinching. In this specific case, it refers to the pinching of the labrum, the edge cartilage between two bones – the acetabulum and the head of the femur. For better understanding, the acetabulum is spherical and continues into a relatively narrow neck, which, in turn, is angled to the acetabulum. This “design” allows for relatively great mobility of the joint while protecting its soft structures. Impingement of the labrum occurs in five different situations:
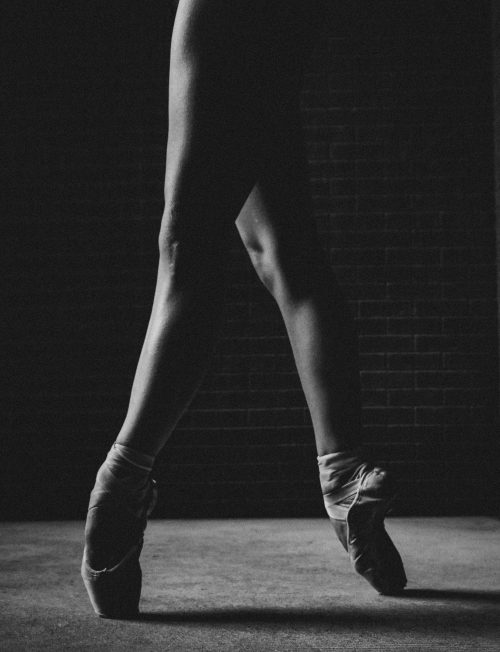
- Normal anatomy, but physical activity encourages extreme movements of the hip, such as in gymnastics or ballet, for example.
- Thickening in the area of the femoral neck, immediately adjacent to the head (also called a CAM lesion) and/or thickening of the acetabular rim (the so-called PINCER lesion), which limits hip mobility and can irritate or damage the labrum during sports activities or prolonged sitting.
- Hip dysplasia, especially of the acetabulum. This means that the acetabulum is shallower than desired, allowing for greater hip mobility, which puts the labral edge under significant stress, especially during sports activities.
- Normal anatomy, but congenital laxity of the ligamentous system. This condition reduces or eliminates the protective role of ligaments and tendons, allowing impingement of the labrum in extreme positions or repetitive movements with high resistance. Such situations are often found in water sports such as synchronized swimming or water polo.
- Two or more of the above disorders in combination.
In any of the described variants, the symptoms include groin pain during specific movements, sports activities, sitting, or after walking or running. The discomfort can be very intense, hindering daily activities, even causing limping and sharp restrictions in hip mobility. In another variant, the symptoms may be mild, more like discomfort when rising from a seated position, a feeling of difficulty in walking, especially uphill or stairs, or mild pain after physical activity.
It is important to note that FAI occurs in younger people, typically up to their thirties, with the first onset of symptoms usually occurring in adolescence. Groin pain after the age of 40 indicates other conditions, most commonly hip arthritis.

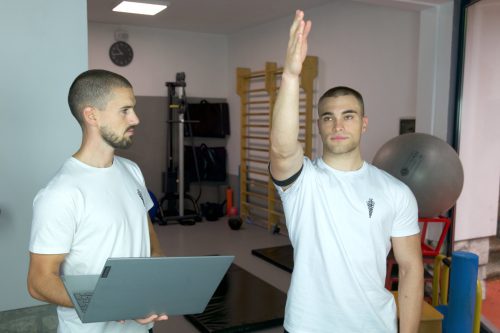
When symptoms persist for more than 7 days, it is advisable to have an examination by an orthopedist or experienced physiotherapist. If impingement is suspected upon examination, X-rays are taken in one or two positions. If changes in the bony shape of the joint are seen on the images, it confirms the diagnosis, and treatment follows. If the X-ray is normal, it is advisable to also have an MRI of the hips to assess the condition of the soft tissues. MRI is also indicated in professional athletes for accurate prognosis and treatment planning, as well as determining the length of time away from sports activities. In adolescents, it is necessary to rule out so-called epiphysiolysis, which has similar symptoms but is treated differently, and in older patients, especially after the age of 30, the possibility of bone edema or osteochondritis dissecans (OCD), which also has similar symptoms but requires different treatment. Inguinal hernia is not uncommon and manifests with similar symptoms, making it easy to suspect during examination, and the patient is then referred for further internal medical evaluation.
When it is certain that hip impingement, with or without labral damage, is present, it is important to start appropriate physiotherapy. The classic approach with electricity, ultrasound, laser, and similar methods that reduce inflammation will not be of great benefit here. As it is mechanically induced damage, treatment must necessarily have a mechanical basis through manual therapy focused on reducing pain and improving the physiological sliding of the joint bodies, which should result in reduced irritation of the soft tissues. After reducing pain, it is extremely important to prevent re-pinch through an individual exercise program aimed at establishing control of movements during daily or sports activities. This process can take weeks or months, depending on the type of impingement, anatomical variants, and the sport the patient engages in.
Tension model
Within the tension model, we view the hip as part of a large mechanical complex that includes the entire lower extremity, pelvis, and lumbar spine, and in sports involving throwing with the arm and the entire spine, together with the shoulder. From this perspective, the need for increased hip mobility will arise if there is a limitation of movement anywhere else in the body, whether it is due to anatomical limitations, habitual (through habit or incorrect running, jumping, shooting technique, etc.), or a protective mechanism due to a previous injury (muscles around the hip, ankle sprains, knee, shoulder, back, etc.). Because of this fact, an examination of existing hip complaints cannot be complete without examining surrounding joints and, if necessary, all joints, including the spine. Only then is it possible to hypothesize about the cause of impingement and create an individual treatment plan, recovery, modification of the training process, correction of identified deficiencies, and gradual return to sports activity or daily life. For athletes, in addition to the clinical examination, a battery of functional tests is necessary (such as balance assessment, tensiometry, muscle strength and endurance measurements, running and jumping techniques, etc.). The absence of this step is the most common reason for repeated complaints or chronic pain that only temporarily subsides after general physiotherapy.
Only when individual physiotherapy with all described components has been performed, which has not led to the desired improvement, which occurs in less than 10% of all impingements treated at our institution, and in agreement with an orthopedic specialist, surgical treatment is planned. Depending on the type of impingement described earlier in the text, such an arthroscopic procedure may involve only repairing the damaged labrum or additional grinding of bone prominences. When performed by an experienced surgeon, this surgical procedure is very successful, complications are rare, and recovery is relatively quick. It is necessary to conduct thorough postoperative rehabilitation guided by the same principles as non-operative treatment and establish prevention mechanisms through regular exercise. Although the damage has been repaired and bone prominences removed, the processes in the body that led to them will be reactivated if desirable movement patterns are not established, both in daily activities and, more importantly, in sports activities under maximum load in terms of strength, explosiveness, and endurance.