It was long believed that every muscle rupture or damage is a trauma. The logic behind this belief was that the pain and the damage occur suddenly, not gradually. Some professionals still adhere to this principle. However, time, experience, clinical practice, and some studies have shown that there are two types of muscle injuries.
Ruptures – muscle injuries, damage and tears
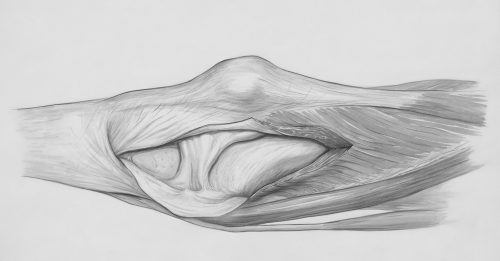
Description
If you suddenly and unexpectedly slip and perform a “split,” a muscle rupture will occur, and it is of a traumatic type. However, if an athlete, after warming up and preparing, experiences the same rupture during a sprint or a sudden change in direction, it is the result of a prolonged overuse process that ended with the same outcome. Similarly, a direct blow to a muscle can cause its damage. In that case, it is also a trauma, but of the contusion type.
But what is the physiological basis for ruptures that occur as a result of overuse? To this day, this remains largely unexplained. Several candidates exist. One is cumulative damage to the internal connective mechanism of the muscle, which provides its strength and helps transmit forces to the bones. This damage occurs similarly to overuse tendon syndromes. When micro-damages in these structures become collectively large enough, they do not cause pain but rather local weakness in force transmission. Thus, even relatively minor loads can lead to significant damage or rupture. Evidence supporting this theory includes the localization of the most common ruptures, which are at the muscle-tendon junction or near the internal connective reinforcements within the muscles themselves. However, there is little direct evidence for this theory.
Another hypothesis is circulatory. It postulates the possibility that parts of the muscle, for various reasons, are poorly supplied with capillary networks, reducing the delivery of nutrients and oxygen. Over time, and under specific conditions, this can lead to a rupture. Supporting this hypothesis is the fact that aerobic training, when included in injury prevention programs, significantly reduces the incidence of these injuries. However, evidence for this theory is also relatively limited.
The third hypothesis combines the first two and introduces another factor into the equation: insufficient dynamic flexibility of the muscle or muscle group. This hypothesis finds its arguments in the biomechanical analyses of injured athletes. However, a significant counterargument is the occurrence of muscle ruptures in ballet dancers. If anyone has good dynamic and static flexibility, it is them. To complicate matters further, there are two types of muscle ruptures (non-traumatic): fast and slow, depending on the conditions under which they occur. In short, it seems that more than one factor influences their occurrence. There are also chronic muscle ruptures.Their diagnosis is simple. Clinical tests (stretching and isometric tests) clearly indicate a muscle injury. Ultrasound examination reveals which part of the muscle is damaged, the extent of the injury, the presence and size of a hematoma, and whether the tendons are intact. Following the diagnosis, therapy begins.
 Simply put, all muscle ruptures start with sudden and sharp pain, which does not subside with rest. Regardless of the type and cause of the injury, the initial treatment is the same for all.
Simply put, all muscle ruptures start with sudden and sharp pain, which does not subside with rest. Regardless of the type and cause of the injury, the initial treatment is the same for all.
In the first 48-72 hours post-injury, it is advisable to rest, apply cold or ice packs to reduce overall swelling and bruising, and use elastic bandages on the injured area to increase intramuscular pressure and thus minimize blood leakage from damaged vessels. During this phase, it is strictly contraindicated to perform any massages, use warm procedures from physical therapy, or engage in any form of training. This is because we aim to allow for the primary healing of blood vessels, reduce the final size of the hematoma, and prepare the muscle for therapy that starts on the 4th or 5th day after the injury.
At this point, a rather aggressive approach begins, consisting of resorptive procedures (warm procedures, radiofrequency therapy, moderate-intensity massage, lymphatic drainage), circulatory training in the form of low-intensity aerobic training, and the first eccentric exercises (click for article) within the tolerable range, i.e., with minimal pain. This approach is novel because, until not so long ago, it was believed that rest accelerates and facilitates muscle healing, and that exercise, especially eccentric exercise, would lead to new injuries. However, a wealth of scientific research, combined with clinical practice, has shown the opposite to be true.
Gradually, over the following days and weeks, local eccentric exercises are intensified first, followed by global ones. Additional parts of training are incorporated as symptoms decrease or disappear. The entire recovery process ends when a full training load can be performed under controlled conditions without pain.
The physiological reasons why this protocol yields better results than mere rest are as follows: better blood and lymph circulation, providing more oxygen and nutrients to repair the damage. Eccentric exercises and aerobic training, even in the early stages, allow the body to form a smaller scar with fibers aligned in the direction of force or stretch, thereby reducing the likelihood of creating secondary points of force disruption within the muscle, which could foster new injuries.
“Breaking up a hematoma” is an age-old procedure still unfortunately practiced by many sports therapists today. It involves very rough massage at the site of muscle injury with the “goal” of spreading the hematoma over a larger interstitial surface (the space between muscles), thereby allegedly speeding up its resorption. However, there is no evidence in professional literature that such an outcome actually occurs. In clinical practice, such procedures do not shorten healing time; on the contrary, they usually prolong it. With a bit of logic, it is clear why this is the case. When traumatized and damaged tissue (whether from external or internal forces) is subjected to rough massage, additional damage is caused—not necessarily to the muscle itself but to the skin, subcutaneous tissue, and often the superficial fascia. Consequently, the body is left to heal multiple injuries rather than just one, resulting in an extended overall healing time. Additionally, the “spreading” of the hematoma to a larger area is anatomically limited by connective tissue sheaths. If this spreading can occur, even mild to moderate massage or specific physical activity can achieve the same result without causing secondary tissue damage.
This procedure belongs to the realm of historical physiotherapy practices and should remain there.
Size of the rupture and healing time
There are two basic types of muscle ruptures: partial and complete. The latter represents a very serious condition, with some cases requiring surgical intervention, while others can be managed conservatively. Partial ruptures can be small or large. Determining what constitutes “small” or “large” is challenging, as experts do not fully agree on this. A common approach is to measure the percentage of muscle fibers affected, such as 20%, 30%, 50%, or more. For example, a 50% rupture may be considered a minor injury if the muscle plays a small role or has many functional assistants (e.g., the hamstring or calf muscles). However, the same 50% rupture in another context, such as the rectus femoris (part of the quadriceps with a crucial role in leg lifting and few assistants), would be a major injury. Similarly, a rupture measuring 2 cm, as detected by ultrasound or MRI, may be a minor injury in the hamstrings but a significant injury in the upper arm or shoulder.
Furthermore, due to the reaction of the surrounding undamaged muscle and the size of the hematoma, assessing the percentage of damaged fibers can be subjective and dependent on the impression and experience of the radiologist or specialist performing the ultrasound. For this reason, radiologists today use one of several protocols for measuring rupture size. Each has strengths and weaknesses, but none predict healing time based on measurement results or protocol interpretation. This estimation inevitably falls on the clinician’s shoulders.
Thus, any estimate of healing speed found in literature or on the Internet is arbitrary, even when based on rupture size. Scientists are aware of this, so most literature focuses on symptom-based recovery and, occasionally, follow-up ultrasound results. Both approaches have their issues.
Pain in partial muscle ruptures decreases and disappears long before the rupture fully heals. Many athletes return to sports activities once the pain subsides, only to reinjure themselves shortly afterward. While ultrasound (and MRI) are excellent tools for diagnosing ruptures and measuring their size, they are less reliable for assessing healing. It is sufficient to note that in most partial ruptures, scars, damage, or irregularities at the injury site may be visible for up to a year post-trauma. They can assist in evaluating healing progress but cannot definitively determine if and when healing has concluded.
As always in clinical practice, we are left with many questions and few answers. By combining scientific research findings with clinical experience, we can create general guidelines to aid both clinicians and patients without access to professional guidance. It is important to note that these are merely frameworks tailored to individual patients since healing speed depends on factors such as whether it is the first or third rupture at the same site, recent ruptures at other locations, the sport involved, the patient’s age, and various physiological and kinematic specifics. With this in mind, here is the general protocol followed by our clinic:
-Muscle strain: All symptoms of a muscle rupture, but ultrasound shows no damage or fiber discontinuity, only minor changes in tissue echogenicity. Estimated recovery time is about 10 days.
-Small partial muscle rupture (up to 2 cm in diameter, in a muscle with functional assistants): If it is the first injury, the estimated recovery time is about three weeks before a gradual return to sports. A second rupture in a short time frame typically requires 6–12 weeks before returning to sports.
-Large partial rupture (over 2 cm in diameter, in a muscle with functional assistants): First injury recovery time is 4–6 weeks. A second rupture at the same site requires 8–12 weeks.
The rationale behind this protocol lies in the previously mentioned fact that we cannot fully rely on symptom disappearance or ultrasound findings to assess healing. Instead, we incorporate healing physiology, its speed as estimated by scientific studies, and other factors discussed earlier. Using this approach, our clinic statistics show a rerupture rate of less than 5% among patients who complete the entire rehabilitation protocol, an excellent result compared to available scientific literature.
Recurrent muscle ruptures
When they occur at the same location, recurrent ruptures are invariably the result of inadequate treatment—usually too short or poorly targeted—combined with an overly rapid return to full training. Additional factors may include chronic injuries, kinematic issues, inadequate general prevention, and other reasons. Treating them requires accurate diagnosis of these factors and a comprehensive approach to their resolution. Otherwise, there is a risk of developing a chronic muscle rupture.
Chronic muscle rupture
This condition involves athletes experiencing symptoms during training even after multiple appropriate treatments for repeated ruptures. These pains may last from a few minutes to several days or may be permanent, appearing with every sprint. What they have in common is that they completely prevent sports participation.
Diagnosis is clinical, based on medical history and examination findings. In some cases, ultrasound or MRI can detect a large scar at the painful site, with or without signs of additional muscle damage resulting from previous injury healing. The exact cause of this condition is not fully understood. Hypotheses range from improper force distribution at the scar site to chronic inflammation or poor local circulation caused by an avascular zone around the scar.
Treatment addresses all these possibilities, focusing on the injury site with three goals:
-Softening the scar and stimulating its remodeling through manual therapy methods, shockwave therapy, and isolated eccentric contractions.
-Stimulating local vascularization through low- or variable-intensity aerobic exercise, laser, and radiofrequency therapy.
-Correcting kinematic deficiencies in the larger kinetic chain of the entire limb through concentric and eccentric coactivation and establishing a desirable movement pattern.
Treatment duration is rarely less than six months.
Myositis ossificans (traumatic)
Muscle injuries heal through scarring, but in some cases, the process does not stop at connective tissue formation and continues to cartilage formation and eventually bone creation. This condition is called traumatic myositis ossificans. Although it can occur in any muscle and with any type of rupture, it is most common in contusion ruptures (caused by a blow to the muscle), particularly in the anterior thigh (quadriceps). It can also result from surgical procedures.
Diagnosis is made through examination and ultrasound. Treatment is similar to other ruptures but with one exception: relative rest and avoidance of intense or aggressive physiotherapy procedures during the first 3–4 weeks after injury, depending on the size and location of the injury.
After this period, the focus shifts to restoring normal muscle function through individualized and specific exercises, supplemented by thermal procedures and manual therapy for myofascial relaxation. Any additional roughness or trauma in the early phases of myositis ossificans can increase the total volume of newly formed bone.
For most patients, including athletes, physiotherapy suffices, and they are ready to return to sports approximately three months post-injury. For severe cases, recovery may take up to six months. Surgery is rarely needed and only considered if physiotherapy fails to yield satisfactory results.